
By Christie R. House
July 3, 2023 | ATLANTA
Chicuque Rural Hospital, situated close to Inhambane Bay in Maxixe, the largest city in Mozambique’s Inhambane province, is considered a rural hospital. Though close to this urban center, it is in a remote area, a place where the road is deteriorating, and access is difficult. But it is also where an average of 94,000 people from four rural provinces come for health care each year.
The Rev. Arlindo Romão, the hospital administrator, takes all this in stride as he seeks to provide the best heath care possible. “Chicuque Rural Hospital is a public hospital unit,” he explained to a reporter, “therefore of the Government of Mozambique. But a legal decree allows capable collective entities to take over a hospital and manage it. It was based on this provision that The United Methodist Church of Mozambique offered to help the government. The hospital is currently under the full management of the UMC.”
The government supports the cost of staff, electricity and water, equipment, medicines and medical supplies as much as it can while the international UMC and other donors assist with service gaps and special projects.
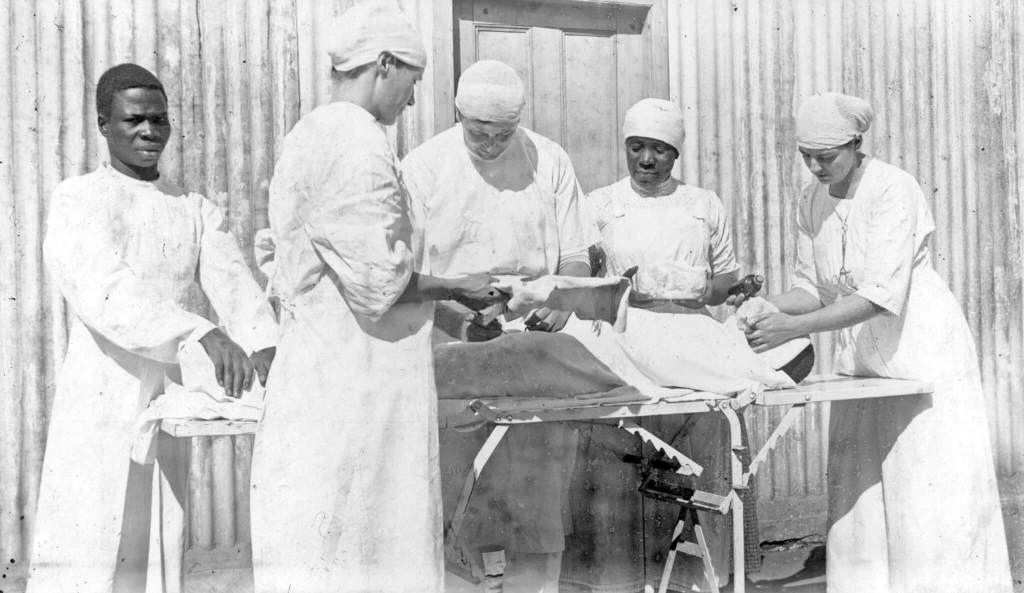
One reason United Methodists of Mozambique offered to do this after the government took over public institutions in 1976 is that the hospital was founded in 1915 by the Methodist Episcopal Church. Dr. Charles J. Stauffacher and his wife, Grace Belkins Stauffacher, arrived as medical missionaries from Wisconsin in 1913. The Stauffachers got to work immediately in Chicuque, making regular rounds also in Cambine and Inhumbane, but Dr. Stauffacher decided the hospital was most needed in Chicuque, Maxixe, where he built the first clinic.
Years are hard on physical structures
While the hospital’s historical legacy gives it rich experience, buildings in Africa’s various climates rarely last a century, and much of Chicuque’s infrastructure has had to be rebuilt. The UMC of Mozambique established a health board to coordinate the work of Chicuque and two other United Methodist health clinics, Cambine, established the same time period as Chicuque, and Maqueze, which was built in the 1980s. The Rev. Maria Matsinhe is the Health Board coordinator.
Global Ministries’ Global Health works with the Mozambique UMC Health Board to fund specific building projects and other facility infrastructure. Over the years, targeted support has been related to malaria; mother, newborn and child health; HIV and AIDS; and water and sanitation needs, all Global Health priorities in African UMC health work.
In 2017, with its proximity to the bay, Chicuque sustained major flood damage from Cyclone Dineo. Currently, the hospital’s emergency unit has been repaired, a new emergency patient alert system installed, and basic furnishings and medical supplies replaced. Going forward, Global Ministries’ has just approved a grant to work on the maternity unit roof and a complete reconstruction of the Expectant Mothers’ Waiting House, where mothers who must travel great distances to reach Chicuque arrange to stay near the time of their expected deliveries.
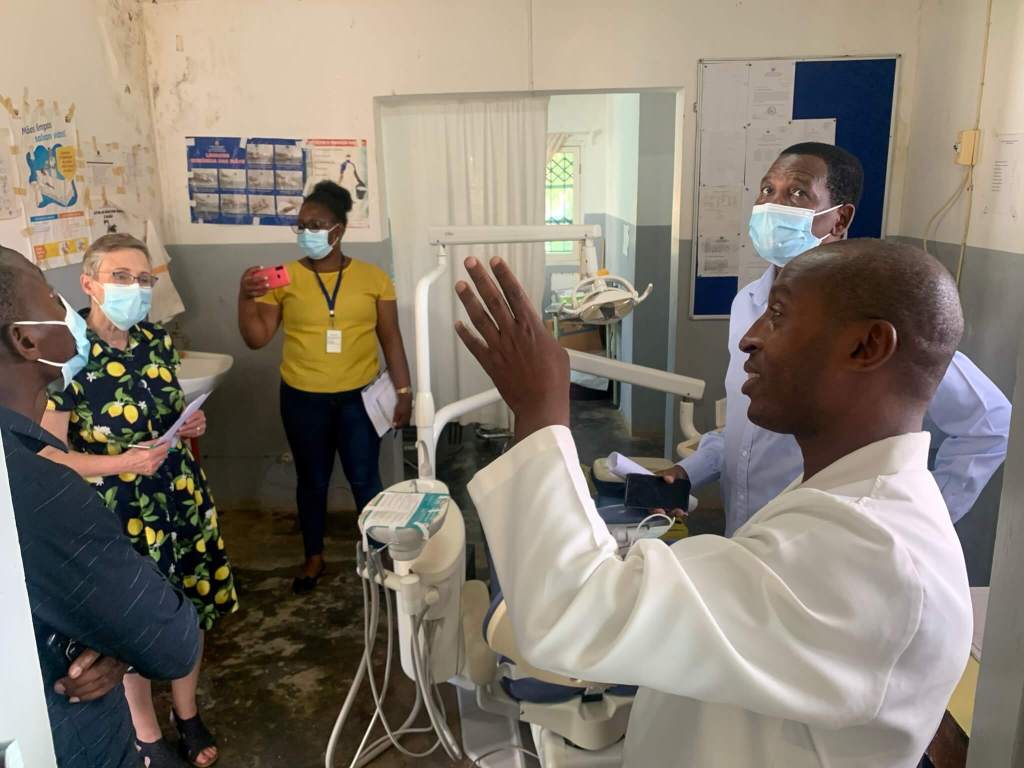
Arlindo Romao. Global Health’s Kathy Griffith looks on. Photo: Elizabeth McCormick
Hospital evaluations conducted by the Mozambique Government in 2023 classified Chicuque as having 100% improvement in infrastructure and meeting 80% of all other markers, though, in many cases, Chicuque was in the 90% range. These results prompted a grant from the World Bank for the hospital and its health center, a separate facility.
Plans for Cambine
Nearly 40 miles from Chicuque is Cambine, another UMC mission with an education center, including 2,000 students at several educational levels, and an orphanage, health center and small farm where innovative food production methods have been developed and passed on to farmers in the community.

The health center offers primary health care and maternal, newborn and child health services. It also has a small inpatient unit for about 20 patients, but the building has needed repair for a long time and the roof damage was exacerbated by Cyclone Freddy’s high winds earlier this year. The health board has been working with the Global Health unit on a 2023 grant to repair this facility as well as other essential buildings, like the Waiting Mothers Home.
The staff are motivated and busy at the health center, organizing regular mobile clinics to help reach those living far from services. One of the midwives is Florence Kaying, a Global Ministries missionary from the Democratic Republic of Congo. She has worked at Cambine and in the community for five years, learning the language, customs and how to impact health behavior while she has consulted pregnant women, delivered their babies and followed-up with care.
Each month, Matsinhe, the Health Board coordinator, calls on the community to own their health facility, asking them to help with general maintenance on the property. Several congregations have also made contributions with cleaning materials.
Maqueze Health Center
While Chicuque and Cambine are on the coastal side of Inhambane province, Maqueze is inland to the southeast in Gaza province, about a six-hour drive away – rural and very busy.
It too has experienced significant storm damage and the building is compromised. A separate corrugated iron room accommodates pregnant women who don’t have access to services closer to their villages, and a third building houses the female nursing staff. There is no doctor. Like the other two health facilities, the health team sees patients with primary health care needs, offers maternal newborn and child health services, and diagnoses and treats malaria. Maqueze is also a treatment center for those with tuberculosis and HIV.
In 2024, the health board will receive a grant to initiate renovations here, including water, sanitation and hygiene interventions. In the meantime, the government offers support through staff, medicines and medical supplies, and the community works at maintenance and care in partnership with the nursing staff.
Though it has been more than a century since Methodist medical missionaries arrived in Mozambique to establish Western-style medical missions and facilities in remote places, health ministries supported by the United Methodist Church save lives and continue to serve some of the most vulnerable populations today. Without them, thousands of people would have no health center in reasonable traveling distance. The dedication and conviction of Mozambican health professionals extends the UMC mission tradition of providing health care for all God’s people.
Christie R. House is a consultant writer and editor with Global Ministries and UMCOR.
Global Health
Methodism’s focus on health as a part of mission dates back to the 19th and 20th centuries when missionaries expanded the options for health care in underserved communities. Today, through United Methodist conferences and health boards, Global Ministries works to strengthen whole networks of health responses, from revitalization of facilities and staff training to building better water sources, developing sanitation facilities and promoting nutrition. Global Health concentrates on eradicating preventable diseases, such as malaria, HIV and AIDS, and COVID-19, and supporting the most vulnerable populations, including mothers, newborns and children.
One way to partner with Global Health ministries is to give a gift to the Abundant Health Advance, #3021770.

