Accessible health care spreads hope in Nigeria

By Christie R. House
Patience Zakari, a young mother in rural Nigeria, was afraid to take her children to a clinic when they were sick with fever. She feared the cost of treatment, given her limited budget, which made it difficult to pay for essentials like food and school fees. She preferred, instead, to go to a local chemist to buy cheaper malaria drugs, but they didn’t always work.
When her infant twins became ill, she feared they would not survive. She found a clinic operated by the Nigerian United Methodist Church that was screening for and treating malaria at no cost to patients. “I, my twins, and my other children received treatment and are well again. Now I no longer fear going to the clinic,” Zakari said.
In Nigeria, United Methodist health facilities in rural areas are working to improve their outreach into the communities they serve. The Nigeria Rural Health Program, operated by the Nigeria United Methodist Health Board, oversees 16 rural health clinics in four annual conferences within the Nigeria Episcopal Area. It also supports Jalingo Hospital, constructed in 2017, thanks to an Imagine No Malaria (INM) Hospital Revitalization grant.
A grant from Global Ministries’ Global Health unit supports the operations required to manage the health board’s country office. This integrated and comprehensive approach to the health needs in Nigeria increases access and improves the quality of services delivered.
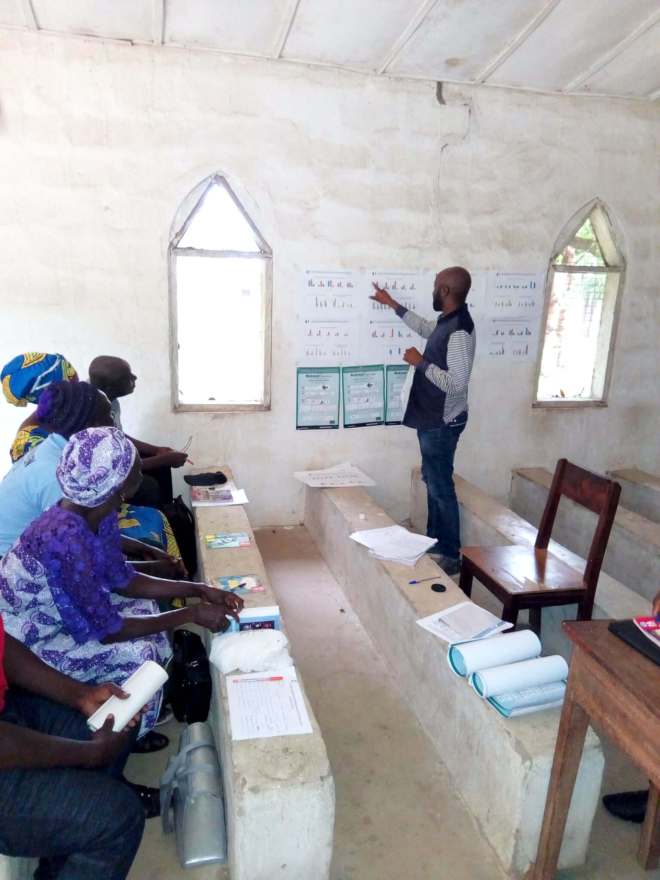
A year-long Imagine No Malaria program provided long-lasting insecticide bed nets, prophylaxis to prevent malaria, and medications and supplies for diagnosis and treatment. Education to encourage behavioral changes to prevent malaria were included in this outreach to community members.
Women who come for prenatal visits receive medication that will protect them and their babies from contracting malaria. They can also be tested for HIV and if they test positive, start antiretroviral medications. With proper treatment, HIV-positive mothers have a good chance of delivering HIV-free newborns.
Marta Sunday, who lives near the United Methodist Taka Wurkum facility, found the malaria treatment she needed after she’d tried others: “I was sick for weeks. Even though I was receiving treatment from another health facility. At Taka Wurkum, within two days, the medication the doctor gave me changed everything, and I am feeling good. My baby is calm and healthy since she was treated in this facility.”
In its first six months, the INM project directly impacted the lives of 21,075 people, including children, pregnant women, and others. More than 2,038 people who might have died of malaria were saved. The project made quality malaria medications available in hard-to-reach communities. And, the number of patients that visited the health facilities where the INM project were offered tripled to 23,991.
The success of this project has boosted staff confidence in the facilities and the level of community trust as well. This trust has gone a long way to increase health, hope and well-being in remote areas.
Give to Abundant Health, Advance #3021770 to support the life-saving work of United Methodist health ministries around the world.
Christie R. House is a consulting editor and writer with Global Ministries.

